Are you curious about your HRA benefit and how to use it? Click here to learn more.
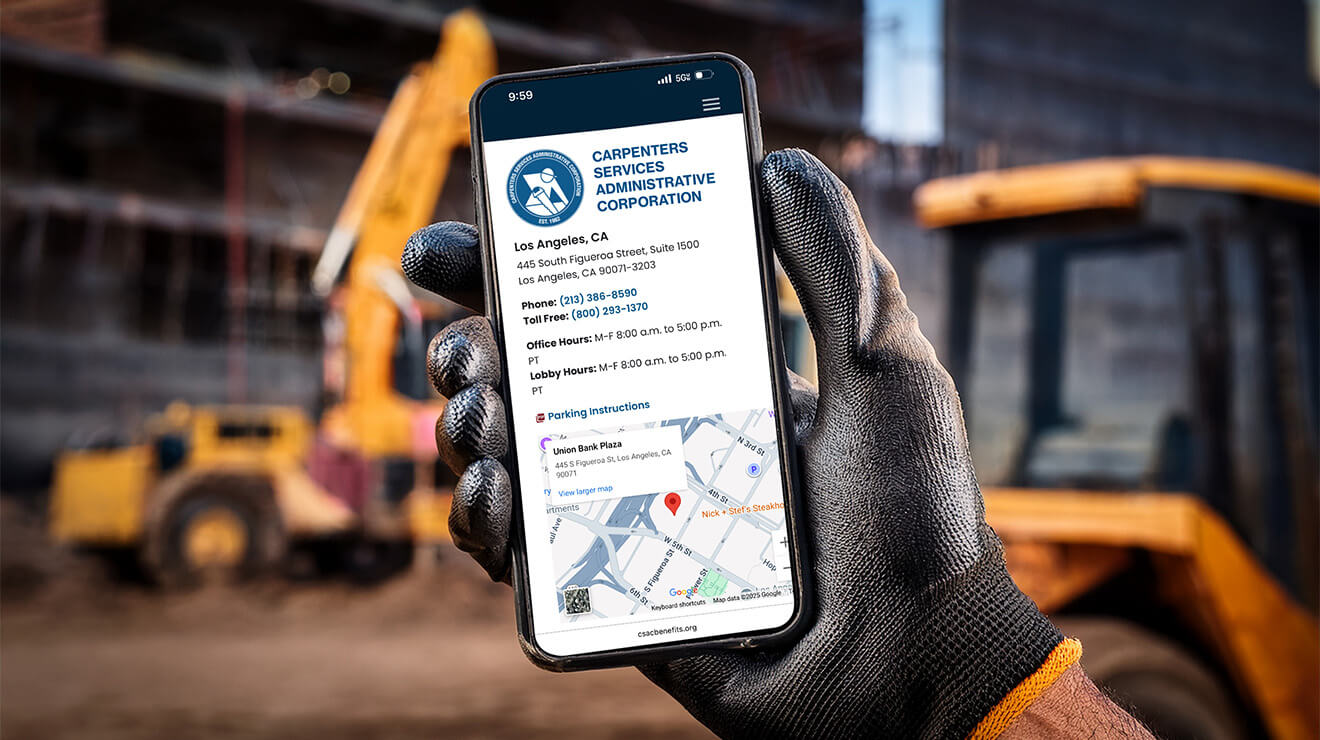
Explore Your Benefits

Retirement
Retirement is not the end of the road; It's the beginning of a new journey.
The Blueprint - Fall 2025
For helpful resources and updates on your benefits, check out the new quarterly benefits newsletter from the Administrative Office.
I Want To...
- locate HIPAA Privacy Notice
- know about Surprise Billing Protections
- download the Participant Information Form
- know how COBRA works
- retire. What do I need to do?
- know how to add and/or drop a dependent.
- learn about new insurance cards from Independence
- access the Southwest Carpenters Reciprocity Form